Welcome to BryLin's Blog
Categories:
Thriving in Business: The Entrepreneur’s Guide to Prioritizing Self-Care by Stephanie Haywood, My Life Boost In the whirlwind world of entrepreneurship, self-care often takes a backseat to the demands of running a business. But here’s the truth: Neglecting […]
Categories:
What is ECT and Is It Covered by Insurance? Electroconvulsive Therapy (ECT) stands as a beacon of hope for individuals grappling with severe depression and other mental health disorders. Recognized by the FDA as a swift and effective […]
Categories:
Unlocking Healing Paths: BryLin Hospital’s Buffalo Mental Health Services In the heart of Buffalo, BryLin Hospital stands as a beacon of hope, dedicated to providing premier mental health services that cater to the diverse needs of the community. […]
Categories:
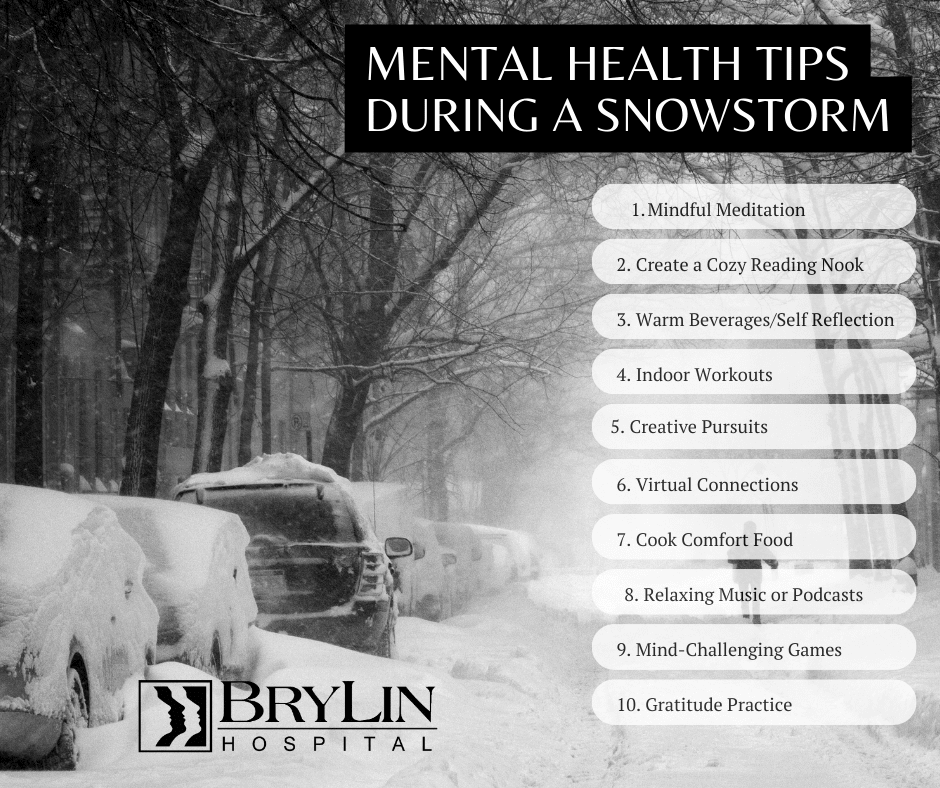
As the snow blankets the world outside, transforming the landscape into a winter wonderland, there’s a unique opportunity to turn a snowstorm into a self-care day. Staying indoors during a snowstorm doesn’t have to be dreary; instead, it […]
The joyous holiday season, filled with festivities, family gatherings, and cheerful decorations, often gives way to a lesser-known phenomenon: post-holiday depression. As the lights dim and the calendar turns, many individuals find themselves grappling with a range of […]
Categories:
Maximize Holiday Joy: 5 Strategies to Minimize Stress and Prioritize Well-Being Embarking on the festive holiday season brings forth a unique blend of joy and challenges. While it’s a time dedicated to family, cheer, and celebration, the myriad […]
November is Men’s Mental Health Awareness Month: Let’s Talk About It November is Men’s Mental Health Awareness Month, a time to raise awareness about the unique challenges men face when it comes to mental health. Men are less […]
Categories:
October is National Depression Awareness Month, and this year, the focus is on depression in children and adolescents. Depression is a serious mental illness that can affect anyone, regardless of age. However, it is especially common in children and […]
Categories:
NCCC Announces 2023 Distinguished Alumni Award Honorees, Student Scholars The Niagara County Community College foundation recently announced their 2023 recipients of their distinguished alumni award. NCCC choose to honor for this year’s award the president of BryLin Hospital, […]
Categories:
BryLin Hospital announced the winners of its inaugural Suicide Prevention Awareness Art Contest at a private awards ceremony on Tuesday, September 26th, 2023 at 1:00 PM. Submissions were accepted in a variety of mediums, including paintings, drawings, and […]